Indicators on Do You Have To Sign Up For Medicare At 65 You Should Know
The smart Trick of Boomer Benefits Reviews That Nobody is Talking About
Table of Contents5 Simple Techniques For Medicare Part GSome Known Questions About Medicare Part C Eligibility.10 Easy Facts About Boomer Benefits Reviews ShownMore About Medicare Supplement Plans Comparison Chart 2021 Pdf

Usage Method B for revenue and properties. Note: If individuals that are additionally eligible for MA satisfy greater than one basis of eligibility, they might select one of the most useful basis for MA, yet must use an Approach B basis for the Medicare Financial Savings Program. Property Guidelines Property restriction is: l $10,000 for a home of one.
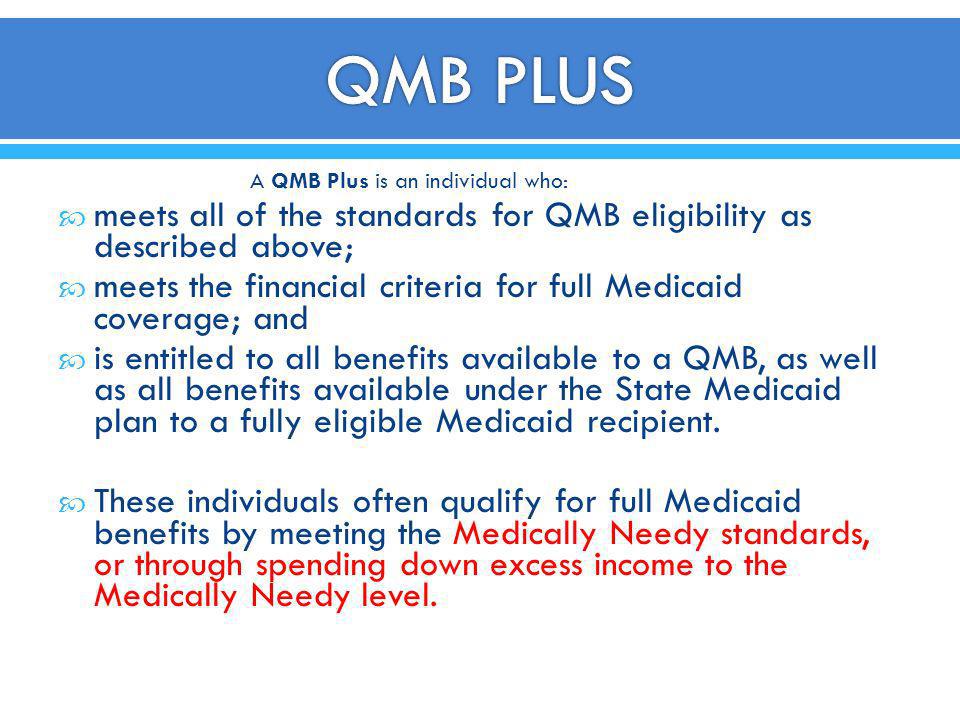
Instance: Bud's income is 125% FPG. He is ineligible for QMB even if he has actually covered costs that would permit him to invest down to 100% FPG. Covered Provider (Prepaid MHCP Handbook) The benefits of the QMB program are: l Repayment of Medicare Component An and Component B premiums. l Settlement of Medicare cost-sharing (co-payments as well as deductibles) for Medicare solutions offered by Medicare-eligible service providers.
It is rarely helpful for people in LTC to be QMB-only due to the fact that: l Medicare Part A covers extremely restricted proficient nursing treatment. l Settlement may not be confirmed till numerous months after the care is received. Nevertheless, if you know Medicare Part A is covering any of the LTCF expenses, it is advantageous for people to be QMB-only because there wouldn't be an LTC spenddown.
More About Medicare Part G
Individuals might receive MA and also QMB concurrently. l Individuals with incomes at or under 100% FPG certify for QMB, and also for MA without a spenddown if their possessions are within MA limits. l Since QMB enables a conventional $20 revenue disregard and MA does not, individuals with incomes over 100% FPG however no even more than 100% FPG + $20 are within the QMB income restriction but have to satisfy a spenddown to receive MA.
Activity: Because Blanche's properties are within the QMB limit but not the MA limit, authorize her for QMB only.
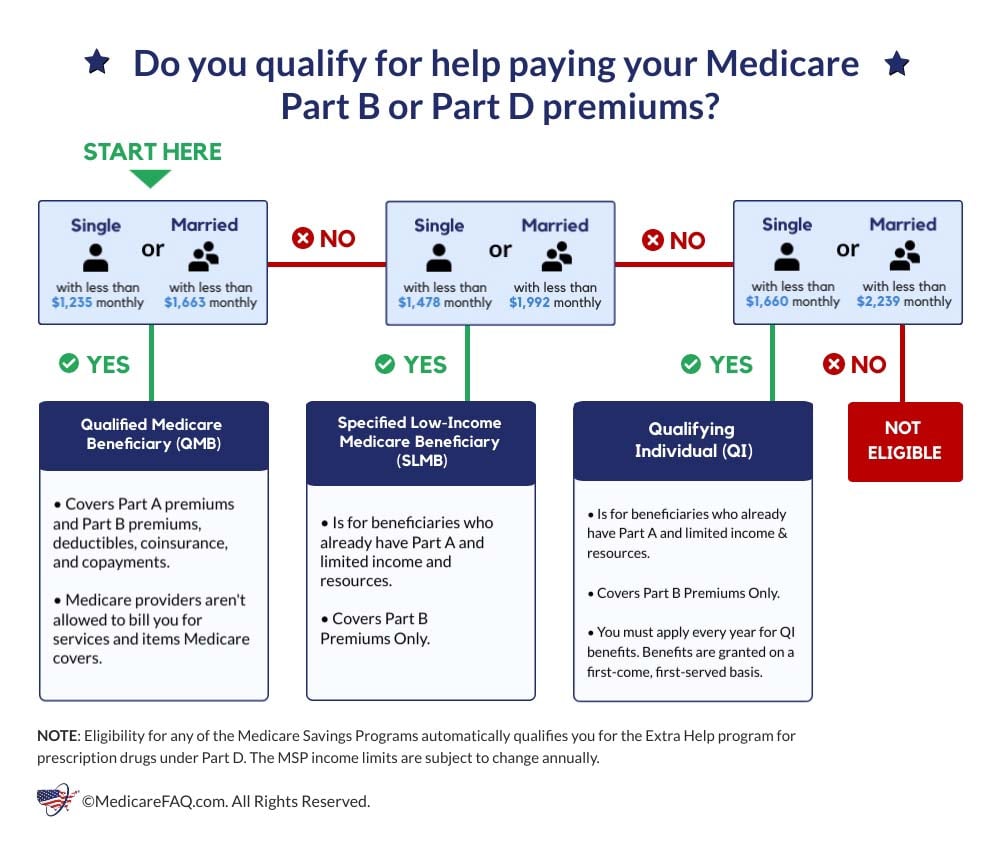
Medicare Cost Savings Programs (MSP) aid people with restricted revenue and resources spend for some or all of their Medicare costs and might likewise pay their Medicare deductibles and co-insurance. There are four various sorts of Medicare Cost savings Programs, this web page concentrates on the Certified Medicare Recipient (QMB) Program. Who Qualifies? If you have earnings from functioning, you might browse around these guys qualify for benefits also if your revenue is greater than the limitations listed.
The Medicare Supplement Plans Comparison Chart 2021 Diaries
Exactly how To Apply Where Do I Obtain These Solutions?
You can likewise go to the Medicare web site to look for Medicare carriers. If you have extra questions about this program please see our Medicare/Medicaid Frequently Asked Concerns or call our Member Call Center. Program Call: , 303-866-5402. The member's benefits are limited to payment of the participant's Medicare Component B costs only. Suppliers must inform the member that the solution is not a Medicaid-covered solution for a member who has just SLMB protection. When the EVS identifies a member as having only Defined Reduced Earnings Medicare Recipient insurance coverage (without likewise having Full Medicaid or Package A protection), the carrier should get in touch with Medicare to verify medical insurance coverage.
When the EVS determines a member as having actually Specified Reduced Revenue Medicare Beneficiary protection and also Full Medicaid or Package A coverage (without waiver obligation), Medicaid declares for solutions not covered by Medicare must be submitted as normal Medicaid cases as well as not as crossover insurance claims. The member's benefit is repayment of the participant's Medicare Component B costs.
The member's advantage is repayment of the member's Medicare Component A costs. The EVS determines this coverage as Professional Medicare Recipient - med supp open enrollment.
9 Simple Techniques For Medicare Part C Eligibility
Annual changes in the FPL suggest that, also if you may not have received QMB in 2014, under the new FPL, you may have the ability to qualify this year. To look for the QMB program, you will certainly need to contact your local state Medicaid office. For even more support, you might wish to call your local State Medical insurance Support Program (SHIP) - medicare supplement plans comparison chart 2021 pdf.
SPAPs are state-funded programs that give low-income as well as medically clingy seniors as well as people with impairments financial assistance for prescription drugs. maoep. We have SPAP information online below (note that the SPAP info undergoes alter without notice): If you do not fulfill the low-income economic needs to receive the QMB program, you still might have several of your Medicare expenses covered by one of the other Medicare Savings Programs.
The FO takes the application as well as refines it according to instructions in HI 00801. 140E.4 of this section. Example of individual requesting Premium-Part An and Component B registration during a registration duration: Ms. Adler lives in Pennsylvania (a Component A Buy-In State) and does not have Medicare. She get in touches with her local FO in January 2018 since she wants Medicare insurance coverage however can't pay for the premiums.
Adler might file an application for "conditional enrollment" in Premium-Part A. Due to the fact that Ms. Adler lives in a Part A Buy-in State, the Component B as well as conditional Part A registration can be filed at any moment. The application is not refined as a General Registration Period (GEP) application. The FO takes the application and also processes it according to directions in HI 00801.